My Latest Lab Results - 065
I'm dedicating today's newsletter to my friend and neighbor Mike, who is a two-time cancer survivor, and who just lost a second sister to cancer. Mike works in the oncology field, is dedicated to his work, and is an inspiration to those who know him.
Lab anxiety
There was the usual low-grade anxiousness in the past two weeks, which is typical for me in the lead-up to getting lab results, specifically, PSAnxiety. It's associated with some low-grade catastrophizing, such as what if I'm anemic or what if the labs suggest bone metastases?
The anxiety is intermittent, but overall, not as severe as it used to be; it still rears its ugly head at test time.
The results
First, the good news. My complete blood cell count (CBC) is normal, and my comprehensive metabolic panel (CMP) is normal, except for a mildly low globulin level. More on the globulin level later.
Testosterone:
Nov 2021: 633 ng/dL
Dec 2023: 870 ng/dL
Jul 2025: 606 ng/dL
And the bad news:
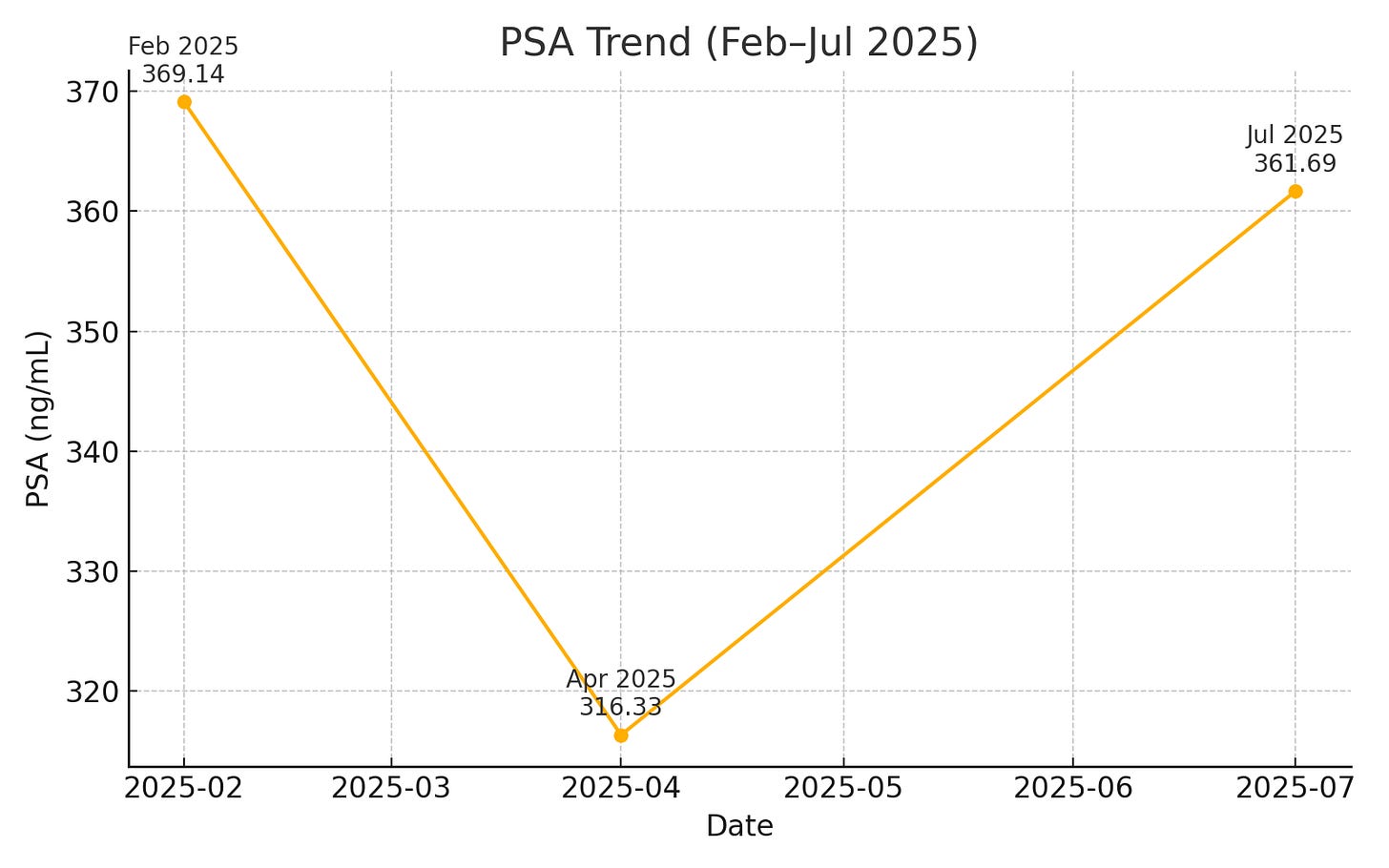
PSA:
Feb 2025: 369.14 ng/mL
Apr 2025: 316.33 ng/mL
Jul 2025: 361.69 ng/mL
My PSA has bumped back up. As a friend put it, "...worst case scenario, your PSA has been level now for six months." That is a good way to look at it.
How did I feel seeing the PSA results? I didn't feel anger, sadness, or fear. I feel a mixture of curiosity, disappointment, and relief.
Curious about why my PSA dropped 53 points and disappointed that it bumped up 45 points. Yet, I'm relieved I don’t have any symptoms or other lab evidence of metastases.
The hardest part was telling Mike, my husband, and seeing him cry. I gave him a tight hug until he stopped crying. After so many years of dealing with this issue, I sometimes forget the stress it places on him.
I'd love to figure out what caused the 53-point drop in PSA so I can take whatever necessary steps to facilitate it.
Analyzing the PSA results
I don't think the PSA drop was due to testosterone in the 600 range, though I have no idea what the testosterone level was in April. Testosterone levels fluctuate with peaks typically occurring between 7 and 10 am, though that diurnal variation appears to be blunted as men age. My labs were drawn closer to noon.
I don't think the prior PSA, which showed a drop, was a lab error because if it were, the current one should be significantly higher than it is. I say that because my PSA had been doubling every 8.4 months from January 2019 to February 2025.
I use Memorial Sloan Kettering's PSA doubling time calculator to track my doubling times.
My lowest PSA ever was 0.9 in January 2019, which was after a radical prostatectomy and salvage radiation to my pelvis. My highest PSA was 369.14 in February 2025, and then it dropped 53 points to 316.33 in April 2025.
The only thing I did differently between February and April 2025 was to start high-dose ivermectin and fenbendazole. And then I increased the dose of ivermectin from 102 mg per day to 136 mg per day and changed the dosing of fenbendazole from 500 mg every other day to 500 mg 7 days on and 7 days off.
If the PSA drop were solely due to the ivermectin and fenbendazole, you would have expected to see a continued drop, not an increase. The problem with viewing things that way is that the body and lab values have numerous variables, making it impossible to account for all of them.
Regardless, there has been a recent significant drop and a subsequent slowing of the doubling time. If the most recent rise in PSA of 45.36 points over the last 3 months remained steady and were multiplied by four, we'd expect a PSA of 497.77 a year from now, which would reflect a much improved PSA doubling time of 18.3 months.
But I'm only speculating.
My point is that something caused my PSA to drop and then slowed the short-term PSA doubling time. Could it be related to the ivermectin and fenbendazole? I cannot unequivocally say these medications caused the April drop or the slower short‑window PSA doubling time.
Correlation doesn't establish causation.
However, it is an extraordinary coincidence that the PSA drop coincided with the start of those medications. If you are a doctor with a traditional view of ivermectin and fenbendazole, you probably rolled your eyes after reading that last sentence.
I understand where you are coming from because I used to do the same thing. However, I'd venture a bet that if you were diagnosed with an incurable cancer and couldn't tolerate the standard of care drug therapy, you'd be exploring all your options, no matter how slim they might appear.
That’s called the will to live, which has served me well since my diagnosis 7.5 years ago.
The low globulin level
The only lab abnormality, other than the high PSA, that stands out is the low globulin level.
In a comprehensive metabolic panel, globulin is a calculated value: total protein 6.4 - albumin 4.7 = 1.7 L (Reference range: 1.9 - 3.7 g/dL). Total protein levels include immunoglobulins (Ig) like IgG, IgM, and IgA.
The low globulin level, or hypoglobulinemia, has been a longstanding issue for me, at first occurring intermittently and now persisting since October 2024. A prior workup with an immunoglobulin panel in 2023 revealed a mildly low immunoglobulin A level, which was normal when later retested.
There are other causes for a low globulin level besides an immunoglobulin deficiency, though my labs don't suggest any of those causes. Even if I do have an intermittent IgA deficiency, there is no treatment for it.
Selective IgA deficiency
Selective IgA deficiency is the most common primary immunodeficiency, but it is highly variable in its expression. Most people are asymptomatic their whole life, while others develop frequent infections such as pneumonia and sinusitis.
Some have highly variable IgA levels ranging from normal to undetectable.
In some individuals, IgA deficiency causes a distortion of microflora in the gut, resulting in an increased incidence of gastrointestinal parasites and small intestinal bacterial overgrowth, which I’ve had before. See More Gut Drama - 034.
Some people with IgA deficiency can show blunting of the small intestinal villi, or lining, which was present on the biopsy of my small intestine in December 2023. Additional testing ruled out celiac disease.
While I have not been formally diagnosed with IgA deficiency, it could help explain some things, like why I had blunting of the villi of my small intestine and why I developed small intestinal bacterial overgrowth.
Gut dysfunction and immune health
I’m discussing this because I’ve recently had a flare of symptoms suspicious for small intestinal bacterial overgrowth (SIBO) - post-meal bloating and intermittent morning loose stools. Sorry - TMI!
When I started training with The Institute for Functional Medicine in 2009, they were well ahead of the curve, teaching the importance of a healthy microbiome for a healthy immune system.
A healthy gut and microbiome are essential for a healthy immune system because the gut-associated lymphoid tissue (GALT) is the largest immune organ in the body. Here is a really good YouTube video explaining the kind of immune functions that occur in the lining of the gut.
Because of this flare of gastrointestinal (GI) symptoms, Dr. Kessler has suggested I undergo stool testing again. While breath testing is the typical way to test for SIBO, obtaining a comprehensive digestive stool analysis gives you a lot more information about the overall function of your GI tract.
When we last did that stool test in the fall of 2023, it showed multiple abnormalities. See Immune Compromised - 028. We addressed each one, and I got better. The problem is that SIBO often recurs, especially in someone with IgA deficiency.
If your gut microbiome is in chaos, chances are your immune system is too. Recent studies have shown the association of the gut microbiome and prostate cancer.
In addition, other studies have shown that immunotherapy for cancer works better when there is a higher diversity of bacteria and a relative abundance of Ruminococcaceae bacteria.
My immune system is probably going to do a better job attacking the prostate cancer cells when my gut is optimally functioning with a healthy microbiome.
The plan
I met with my radiation oncologist and we discussed the lab results. Here is the plan:
I will continue the ivermectin and fenbendazole for now, as I'm not having any side effects or liver enzyme elevation.
My primary care provider will order a serum protein electrophoresis to assess the type of proteins in my serum and another IgA level.
We’ll hold off on a PET/CT scan for now since I’m asymptomatic and all other labs are normal.
I’ll order another Genova Diagnostics’ comprehensive digestive stool analysis to see where we stand with my overall gut function.
If the SIBO symptoms persist, we’ll treat empirically for that.
I’ll continue my current supplement regimen and intensive self-care.
I’ll follow up with my radiation oncologist in three months with labs.
I remain optimistic as we continue working to piece everything together in an effort to strengthen my immune system and keep the cancer under control.
Until the next newsletter, I wish you good health.
Much love,
Keith
Disclaimer
While preclinical research has shown some intriguing anti-cancer properties of drugs like ivermectin and fenbendazole, there is currently no high-quality clinical evidence proving their safety or effectiveness in treating cancer. As such, any claims suggesting that these drugs are effective cancer therapies are not supported by randomized controlled trials or regulatory approval. Fenbendazole has documented drug‑induced liver injury in self‑medicating patients.
This Substack is intended solely for educational and informational purposes. This information is not intended as medical advice or a recommendation for any specific treatment. I do not endorse or advise the use of any drug discussed here, including those I may personally choose to take. Always make medical decisions in consultation with a qualified healthcare professional.



Sending good thoughts. It's time for my quarterly PSA test as well... I would love to know what a T level of 600 feels like. My last test was in the low 300s...
Thanks for sharing!