My PSA Doubling Time Has Drastically Slowed - 069
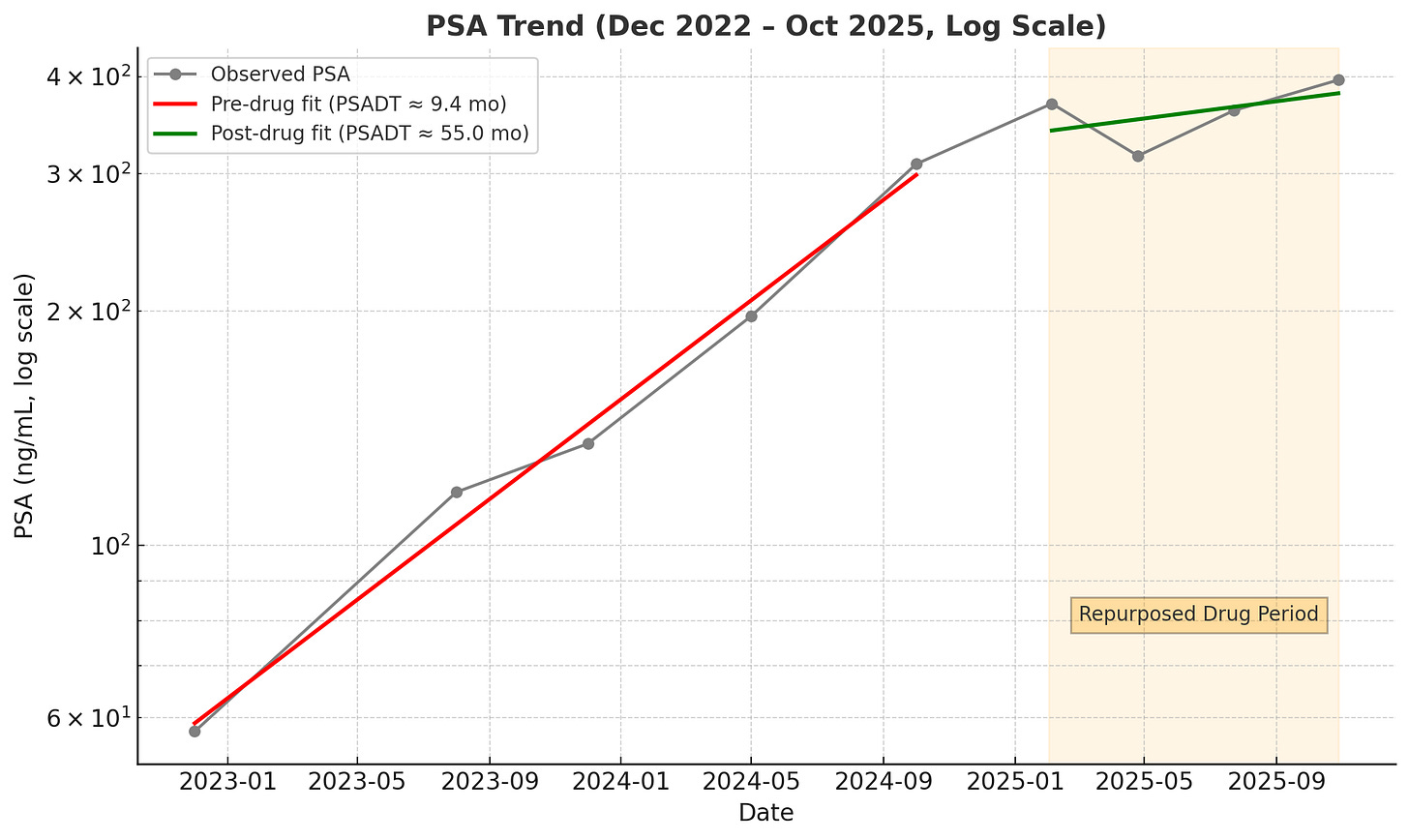
For seven years, my prostate cancer grew at a rapid rate with a prostate-specific antigen (PSA) doubling time (PSADT) of just 9 months.
A short PSADT is a grim predictor, strongly associated with metastasis and mortality.
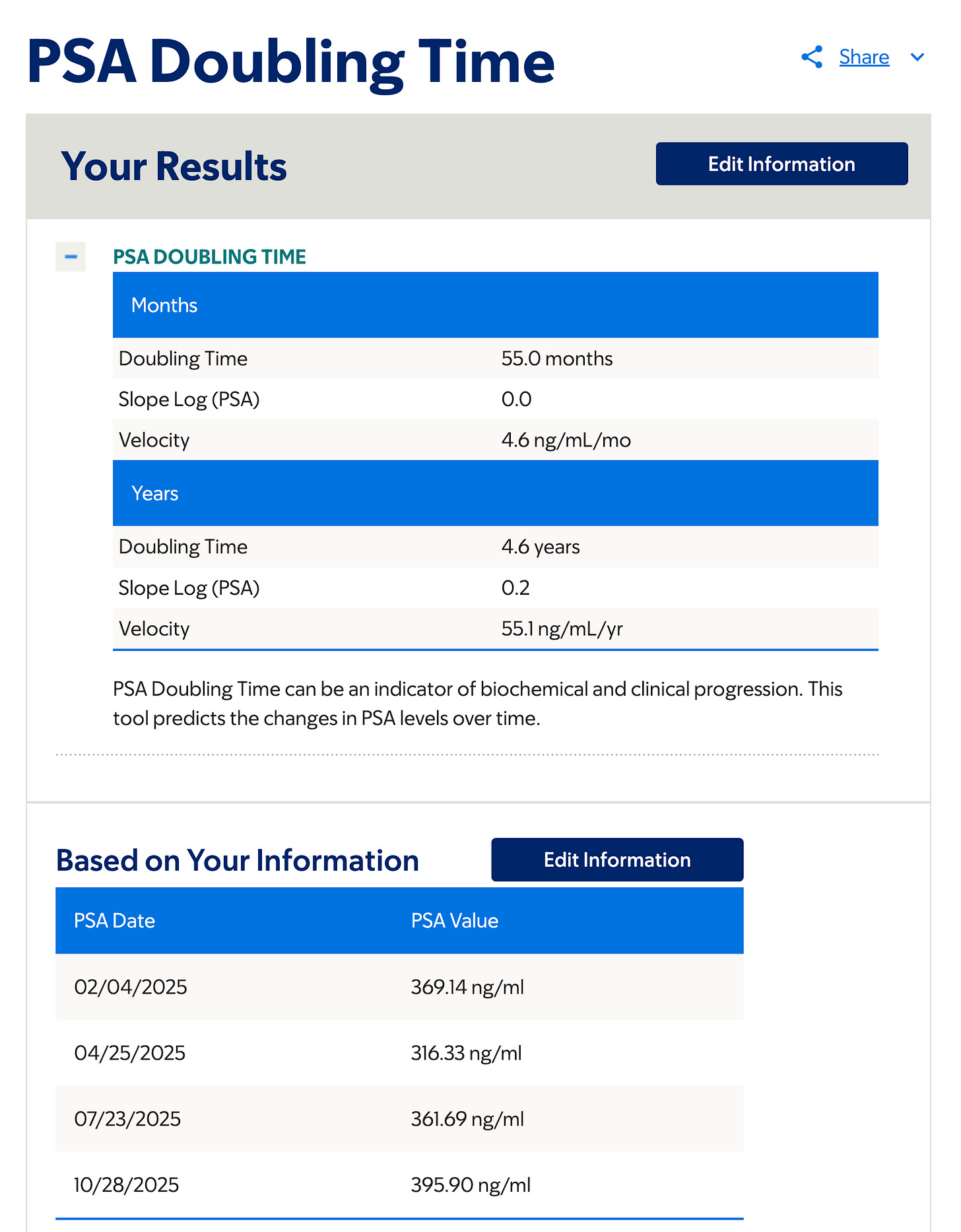
Over the past ten months, my PSADT has slowed to 55 months. That’s 4.6 years!
From Memorial Sloan Kettering’s PSA Doubling Time Calculator
This drastic slowdown began after I started a personal experiment with repurposed drugs.
Prostate-specific antigen (PSA) doubling time (PSADT) is the time it takes for the PSA level to double, reflecting the rate of prostate cancer growth.
A shorter PSADT after definitive therapy, like prostatectomy and radiation, is associated with a higher risk of prostate cancer metastasis and death.
Disclaimer
This post is not medical advice.
There are no clinical trials that have proven Ivermectin, Fenbendazole, or Mebendazole are clinically effective for treating cancer.
However, there are some preclinical data from animal studies and cell experiments that suggest these drugs may have anticancer properties.
My report is purely anecdotal and not a clinical research account.
However, anecdotal case reports are published in peer-reviewed journals because they can document novel treatment approaches and new insights that may one day inspire a clinical trial.
Why I’m rehashing how I got here
To help you understand why the 55-month number is so remarkable, I need to provide a summary of what has happened over the past eight years.
I’m also doing this because I don’t expect new subscribers to go back and read all sixty-eight posts I’ve previously written.
A high-risk tumor profile
In November 2017, after many months of prostatitis symptoms and a PSA soaring to 47 ng/mL, a 60-core biopsy revealed aggressive Gleason 4+3=7 cancer in nearly every sample.
In April 2018, I underwent a robotic radical prostatectomy. I hoped we had caught it in time, but the pathology report delivered a harsh truth.
The cancer was staged pT3b N1. It had broken through the prostate capsule, involved 70% of the gland, invaded both seminal vesicles, and spread to two of nine lymph nodes. The surgical margins were positive for tumor cells.
To make matters worse, the pathology report showed a “tertiary pattern 5,” which is a sign of aggressive disease. This finding indicates that a Gleason pattern 5 was present but accounted for less than 5% of the tumor volume.
My post-surgical PSA didn’t drop to undetectable. It only fell to 4.8 ng/mL.
Genetic testing confirmed the grim outlook:
DECIPHER Test: 0.81 (High-Risk)
Foundation One genomic test: Loss of a key tumor suppressor gene - PTEN - associated with aggressive progression
Intolerance of androgen deprivation therapy
I began androgen deprivation therapy (ADT) in June 2018 with Trelstar. The side effects were immediate and unbearable. Severe hot flashes, drenching night sweats, and profound sleep deprivation led to a deep depression.
I was barely functioning, and I felt like giving up. I made the hard decision to stop ADT after only two injections.
Radiation therapy
In the fall of 2018, I underwent intensity-modulated radiation therapy (IMRT) to the prostate bed and pelvic lymph nodes. However, we were shooting in the dark because a PET scan showed no detectable cancer despite an elevated PSA.
My radiation oncologist felt it was best to radiate where the cancer most likely was.
For a time, it worked. My PSA dropped to 0.9 ng/mL by January 2019.
However, it then steadily began to rise.
My PSA continues to rise
The initial rise in PSA was pretty rapid:
May 2019: 1.72 ng/mL
June 2019: 2.4 ng/mL
July 2019: 3.0 ng/mL
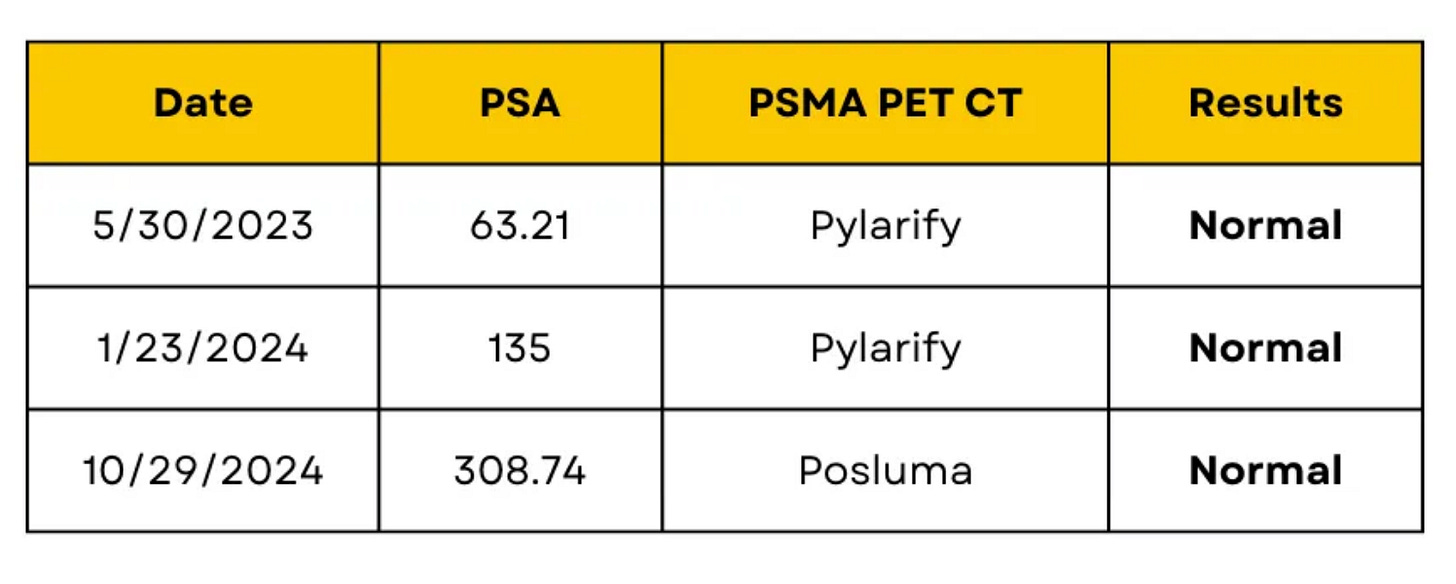
In late 2019, a PSMA PET scan at UCLA showed no visible disease. But my PSA kept rising:
March 2020: 7.3 ng/mL
September 2020: 9.9 ng/mL
April 2021: 20.5 ng/mL
I had an Axumin scan in April 2021, which reported evidence of malignancy in the prostate bed, later determined to be a false positive finding.
I underwent another PSMA PET scan at UCLA. This time, it lit up as small spots in several lymph nodes in the para-aortic chain and pelvis.
My PSA continued climbing:
November 2021: 33.3 ng/mL
March 2022: 41.1 ng/mL
August 2022: 57.7 ng/mL
October 2022: 54.7 ng/mL
December 2022: 57.64 ng/mL
Another PSMA PET in December 2022 confirmed small tumors in six para-aortic lymph nodes and one near the left common iliac node.
Another round of radiation
I underwent proton therapy in January 2023, painting the para-aortic lymphatic chains and “boosting” radiation to the seven small tumors.
Three normal PET scans
Then something remarkable happened. I had three PSMA PET scans in a row, which showed no evidence of cancer despite a rising PSA.
Pivotal decision
In February 2025, my PSA continued to rise to 369.14 ng/mL, and I was forced to make a pivotal decision.
I was now two years out from my last treatment, fighting a cancer that was biochemically raging but invisible to our best scans. I felt I had to do something, but I was not going back on ADT.
On February 13, 2025, I took a different path. I began an experimental protocol of repurposed drugs and supplements:
Ivermectin 34 mg daily
Fenbendazole 500 mg twice daily
Curcumin 3.5 grams daily
Methylene Blue 13 mg twice daily
My PSA takes a dramatic drop
By the end of April 2025, for the first time in years, my PSA dropped 53 points to 316.33 ng/mL.
I increased the Ivermectin to 136 mg daily, keeping the other agents the same. However, by July, the PSA had risen 45 points to 361.69 ng/mL.
Experimenting with repurposed drugs
That’s when I switched the Fenbendazole, a veterinary drug, to Mebendazole 100 mg twice daily and began experimenting with pulse dosing Ivermectin every three days at a very high dose.
After a while, and to no surprise, I developed signs and symptoms of Ivermectin toxicity, and had to back off the dose. I also stopped the Methylene Blue, but I’ll save those details for another Substack post.
I’m not reporting my current pulse dose of Ivermectin as I don’t want others following my footsteps and taking risks without strict medical supervision.
Back pain
In September, I developed unrelenting back pain. My radiation oncologist ordered an MRI scan of the thoracic spine. There will undoubtedly be metastases on this scan.
Nope! It showed no metastases, just multilevel small disc herniations.
After almost eight years of living with advanced prostate cancer, which typically metastasizes to the bone, I have no evidence of any bone lesions despite a high PSA.
That is a miracle!
It seems the repurposed drugs may be working
My latest PSA level, as of October 28, 2025, is 395.90 ng/mL. This time, it rose only 34 points over three months, despite a rise in my testosterone level from 608 to 773 ng/dL.
A rise in testosterone should, in theory, fuel prostate cancer. Instead, my PSADT has stretched from 9 months to 55 months.
There is a pattern here in my numbers since starting these repurposed drugs. A pattern that even the most average physician could see.
It is tough to explain away these findings as chance, especially with the most recent testosterone rise of over 100 points.
The experiment of one
Nearly eight years since my diagnosis and intolerant of the mainstay therapy for prostate cancer—androgen deprivation—I’m still here. Not only am I still here, I’m thriving.
What I write here is not medical advice. It’s my story of walking a tightrope between science, faith, and personal experimentation.
When I started this Substack four years ago, I had no intention of taking experimental repurposed drugs, much less writing about that experience. Yet, this is the path that has opened for me.
My story doesn’t promise easy answers. But it does offer information that one day, I hope, may inspire a clinical trial for men with advanced prostate cancer.
I am not the grim prediction written in a medical textbook.
I am a human being with a name, a heart, a purpose, and a profound will to live.
Most importantly, I’m holding on to and acting on hope.
Conclusion
My radiation oncologist is very intrigued by what is happening. I know I chose the right doctor because he isn’t discouraging or shaming me. He’s curious and supportive.
That’s because he knows who I am - an intelligent physician who does his research and understands the calculated risks I’m taking.
I hope your doctor knows who you are, too.
Since I remain asymptomatic and my other labs are stable, we’re continuing this path and will recheck everything in three to four months.
Until the next newsletter, I wish you good health and much love.
Keith
A Necessary Note: This Substack is intended solely for informational purposes. This information is not medical advice or a recommendation for any specific treatment. I do not endorse or advise the use of any drug discussed here, including those I may personally choose to take. Always make medical decisions in consultation with a qualified healthcare professional.



This disease is wild. You would be dead if you had done ADT up to now with that number. I'm 30+ months on it with Nubeqa and I have Manières and the vertigo this week with the shot, a cold and a cold front has pushed me to the edge. PSA .04 Testosterone 3. I feel wonderful Keith. I'm looking to take a vacation soon.
Great post here Dr. I am just beginning this journey -63 years old - having been diagnosed OCT 2025 with Gleason 8 localized prostate cancer. Just got Decipher test results back scoring .82 (high risk of metastasis). Started repurposed med protocol Jan 7, 2026. PSA has gone from 8.7 in JUN 2025 to 5.1 on JAN 27, 2026. I changed my diet and started focusing on my “metabolic function”. Thank you for sharing your story- there is such a whirlwind of information to process to make decisions moving forward. Presently searching for oncologist in N Florida area that will journey with me since I am not jumping at the traditional treatment options offered.