Liquid Biomarkers Guide Smarter Prostate Cancer Screening- 060
You’re sitting across from your doctor, and you've just been told your prostate-specific antigen (PSA) is elevated. You feel OK with no symptoms. But now you're facing a possible prostate biopsy — a procedure that, while necessary in some cases, carries risks you're not sure you want to take.
What if there was another way to understand what's really going on inside your body, something other than PSA alone?
There is.
It's called liquid biomarker testing, and it's changing the way we think about prostate cancer screening.
Why just a PSA isn't enough anymore
PSA (prostate-specific antigen) is a protein made by the prostate. When it is high, it may mean prostate cancer. However, it can also be high due to benign conditions like an enlarged prostate (BPH) or an inflamed prostate (prostatitis).
Most men with an elevated PSA don't have clinically significant prostate cancer — the kind that actually needs treatment. So, while PSA is a helpful starting point, it lacks precision.
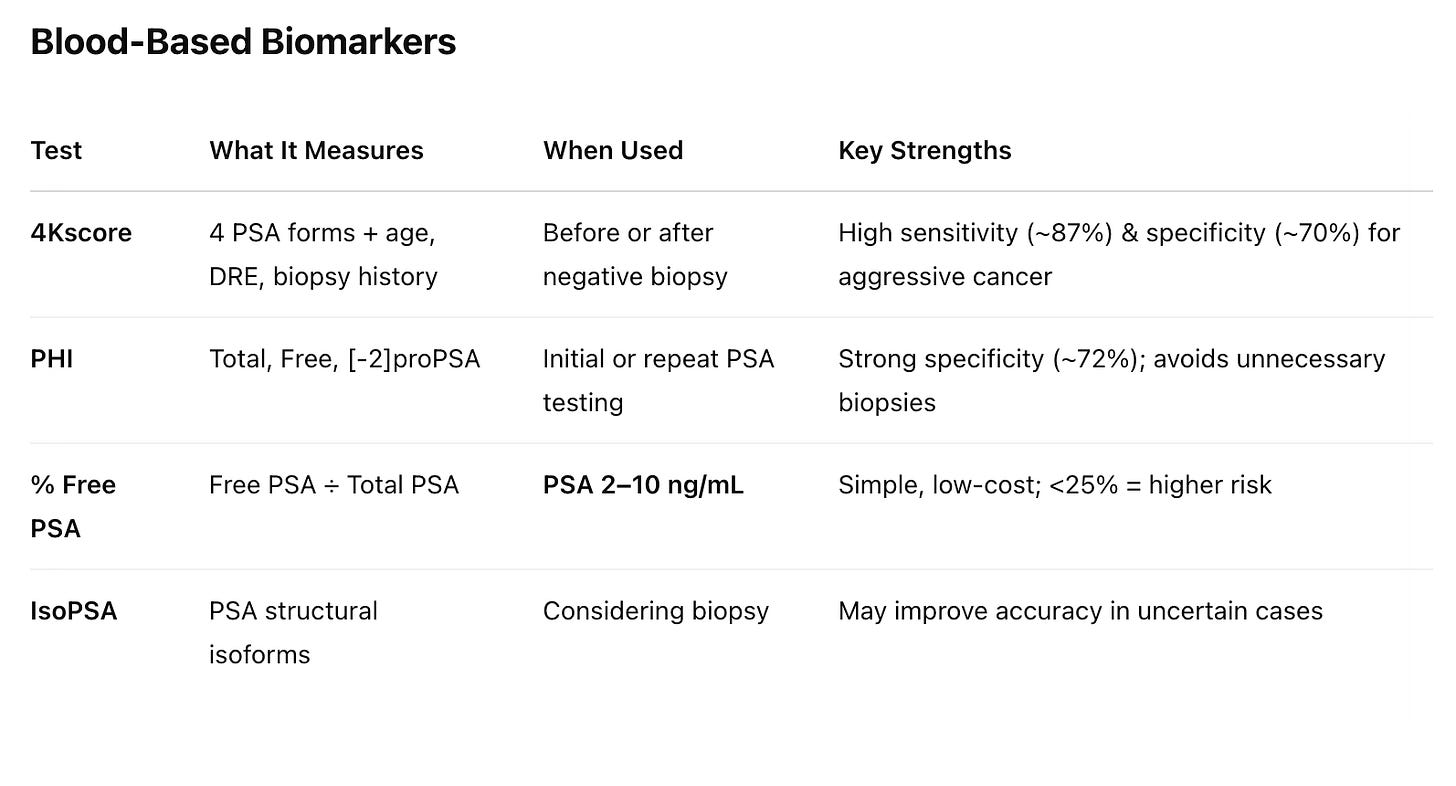
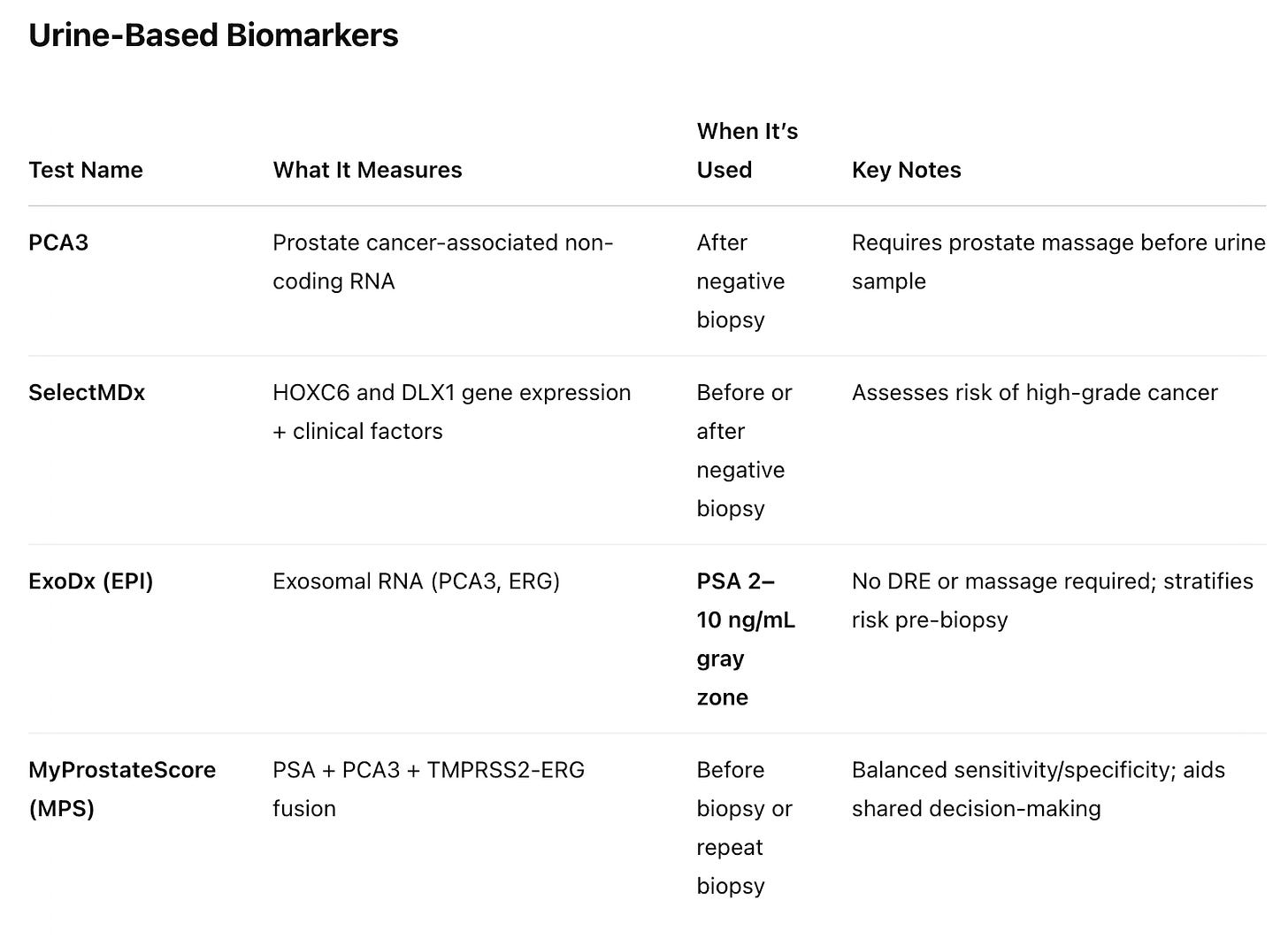
That's where liquid biomarkers come in. These blood or urine tests add detail to the PSA picture, helping to answer whether we need to act right now or can safely wait and watch.
What the guidelines say
Both the National Comprehensive Cancer Network (NCCN) and the American Urological Association (AUA) recognize the value of using multiparametric magnetic resonance imaging (mpMRI) or a validated biomarker, and sometimes both, to refine biopsy decisions.
So, how does this look in practice?
Step 1: PSA is high.
Step 2: A biomarker may be ordered before any biopsy, specifically when MRI access is limited or the MRI results are equivocal.
Step 3: If either a liquid biomarker or mpMRI shows high risk or if both are borderline, you might then proceed to biopsy.
Some experts argue for a liquid biomarker-first approach, especially in men with PSA in the gray zone (2–10 ng/mL), to reduce anxiety and avoid an unnecessary MRI or biopsy.
Others favor doing an mpMRI first, especially in practices with easy MRI access or in men with prior biopsies. The reality? There's no one-size-fits-all. What matters most is combining these tools thoughtfully to personalize your care.
A Simplified Approach
For the average urologist, probably the most straightforward approach is:
Obtain a detailed family history to help stratify risk for prostate cancer. Consider discussing germline testing in men with high‑risk family history per NCCN.
Always repeat the PSA after considering any factors that may have caused or contributed to the high reading.
Wait an appropriate amount of time before repeating PSA testing.
Always add a percent-free PSA with repeat PSA testing. Lower is better, with a 25% or less cutoff of free PSA recommended for patients with PSA values between 4.0 and 10.0 ng/mL.
If the PSA remains high, obtain a mpMRI of the prostate and ensure the radiologist calculates the PSA density by dividing the PSA level by prostate volume. A PSA density >0.15 ng/mL/g suggests a higher cancer risk.
By this point, most urologists will have enough information to help patients make informed decisions about whether to proceed with a prostate biopsy. If there is still a question of whether to biopsy, that's the time to consider using NCCN-recommended liquid (blood or urine) biomarkers.
Access Isn't Universal
One challenge is that not every physician is familiar with all these tests. Clinicians often learn about them through industry reps, conferences, or continuing education courses.
That means they might feel confident using just one or two tests they've worked with before. In addition, insurance coverage varies widely.
Some insurers cover tests like the PHI or 4Kscore. Others may not, or require prior authorization or documentation that the test will change management.
That's why having an open conversation with your treating physician is crucial. You may find that the test you're most interested in isn't accessible, but a similar one is. What matters most is that the test is used in the proper context to guide thoughtful, personalized decisions.
Conclusion
An elevated PSA is just the opening bell. Liquid biomarkers and, where available, mpMRI let you target biopsies at cancers that matter, spare men from unnecessary procedures, and bring genuine precision to prostate cancer screening.
If your doctor hasn’t mentioned liquid biomarkers or an mpMRI, ask about them. The conversation may be the difference between an unnecessary biopsy and the early detection of a cancer that deserves immediate attention.
Understanding your options helps you make better-informed decisions, which is always good.
Until the next one, I hope you stay healthy.
And much love,
Keith
References:
Kawada et al. "Diagnostic Accuracy of Liquid Biomarkers for Clinically Significant Prostate Cancer Detection: A Systematic Review." European Urology Oncology, 2024
NCCN Clinical Practice Guidelines in Oncology – Prostate Cancer, Version 4.2024
Liu et al. "Liquid Biomarkers in Prostate Cancer Diagnosis." World Journal of Men's Health, 2025
Vickers & Lilja. "Five Things You Need to Know About Prostate Cancer Diagnostic Tests." Asian Journal of Urology, 2024
Disclaimer: This post is for informational purposes only and does not constitute medical advice. Always consult with your healthcare provider for any health concerns or before making any decisions related to your health or treatment.


What about the MCED Galleri test from GRAIL? It seems to have a high sensitivity and specificity for prostrate as well?
https://ramkrishnan.substack.com/p/detect-cancer-early-using-blood-biopsy